In today’s era of evolving relationship norms and greater sexual freedom, discussions around se#ual health have never been more essential. While casual dating and multiple se#ual partnerships are increasingly normalized, the potential risks associated with these behaviors—particularly the transmission of human papillomavirus (HPV)—are often overlooked. HPV is among the most common sexually transmitted infections (STIs) globally, yet awareness of its impact on men remains limited. Understanding HPV, its transmission, and the strategies to protect oneself is crucial for safeguarding both personal health and the well-being of sexual partners.
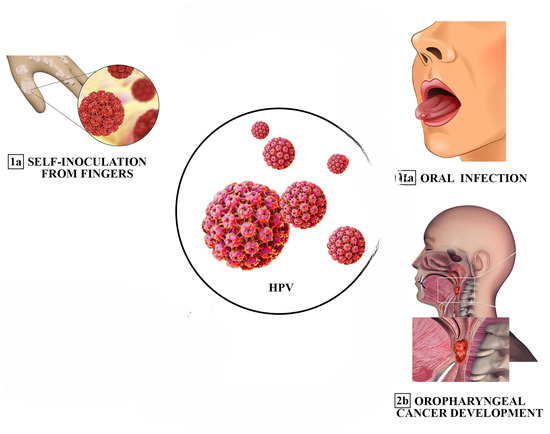
HPV is a group of over 200 related viruses, with around 40 of these strains primarily transmitted through direct se#ual contact. While many HPV infections are harmless and resolve naturally, certain high-risk strains can cause significant health problems. In women, HPV is widely known for its connection to cervical cancer. However, men are not immune. Infections can lead to genital warts and, in more severe cases, cancers of the penis, anus, and oropharynx. Men with multiple female partners face a higher likelihood of exposure to HPV, making proactive awareness and prevention essential.
HPV spreads primarily through skin-to-skin contact during vaginal, anal, or oral sex. Unlike infections that require the exchange of bodily fluids, HPV can transmit even without penetration. This characteristic means that protective measures such as condoms, while valuable, do not offer full protection. The virus can also be transmitted by individuals who show no visible symptoms, making early detection challenging. Asymptomatic carriers can unknowingly spread HPV to partners, underscoring the importance of education, vaccination, and routine health checkups.
A significant factor influencing HPV risk is the number of se#ual partners. Research consistently demonstrates a clear correlation between higher partner counts and greater likelihood of infection. Men who engage with multiple female partners are statistically more likely to encounter someone carrying a high-risk strain of HPV. Each new partner represents a potential exposure, and repeated contact with different individuals can increase the probability of persistent infection. While a single encounter may not pose significant risk, repeated exposure over time can overwhelm the immune system’s ability to clear the virus effectively, resulting in long-term health implications.
Most healthy individuals are capable of clearing an HPV infection within approximately two years. However, repeated exposure to different strains—particularly in a short time frame—can compromise the immune system’s ability to suppress or eliminate the virus. Persistent infections in men are associated with more serious consequences, including the development of genital warts and cancers in the penis, anus, and throat. Symptoms, when they do appear, may include small growths or bumps in the genital region, warts in the airways causing breathing difficulties, and, in rare cases, cancers linked to high-risk HPV strains. Many men, however, remain entirely asymptomatic, which can perpetuate unintentional transmission.
Beyond physical health, an HPV diagnosis can have psychological effects. Men may experience shame, guilt, or anxiety, particularly if they inadvertently transmitted the virus to a partner. Reducing stigma through open communication, education, and awareness is critical for managing both emotional and medical consequences. Understanding that HPV is common and often manageable can help alleviate unnecessary worry and encourage responsible se#ual health practices.
Even men in monogamous relationships must recognize the risks associated with HPV. Because the virus can remain dormant for months or years, individuals may test positive long after a previous encounter. This delayed onset can result in transmission within seemingly committed relationships, highlighting the importance of proactive health strategies regardless of current relationship status.
Preventive measures are key to reducing the risk of HPV transmission. Limiting the number of sexual partners is one of the most effective strategies. Fewer partners reduce the likelihood of encountering high-risk strains and simplify se#ual health management. Consistent use of protection, including condoms and dental dams, also significantly lowers transmission risk, although it does not eliminate it entirely. Vaccination offers additional protection; boys as young as 11 or 12 are recommended to receive the HPV vaccine, and adults up to age 45 can benefit, especially if they are sexually active with multiple partners. Vaccines such as Gardasil 9 target the strains responsible for most genital warts and HPV-related cancers.
Regular health checkups, open communication with partners, and self-education are also essential. While there is currently no approved HPV test for men outside of clinical trials, routine STI screenings and consultations with healthcare providers help maintain overall sexual health. Visual inspections can detect genital warts, and healthcare professionals can provide guidance on managing symptoms or assessing cancer risk.
Several misconceptions surround HPV in men. Some believe only women need to worry about the virus, yet men can experience HPV-related cancers and actively transmit the virus. Others assume that HPV affects only individuals with numerous partners, but anyone who is sexually active is at risk. Additionally, asymptomatic individuals can still carry and spread HPV, making proactive measures vital for everyone, regardless of perceived risk.
If exposure to HPV is suspected, it is important not to panic. Most infections resolve naturally without causing serious health problems. Medical advice should still be sought for treatment of visible symptoms, cancer risk assessment, or vaccination if not previously administered. Timely intervention, responsible sexual behavior, and informed choices create the best defense against HPV.
Living with HPV, when managed responsibly, need not disrupt one’s health or relationships. The majority of infections clear on their own, and complications can often be prevented through vaccination, protection, and monitoring. By staying informed, maintaining open communication, and reducing risky behaviors, men can significantly reduce the likelihood of long-term consequences while protecting both their own health and that of their partners.
Ultimately, the normalization of multiple se#ual partners in modern dating culture comes with undeniable risks. HPV is a silent yet consequential virus for men, and ignoring it does not prevent transmission or health complications. Awareness, education, and proactive prevention are crucial to responsible sexual health. Men who understand the connection between sexual behavior and HPV exposure are better equipped to make informed choices, safeguard their well-being, and maintain healthy relationships.
By adopting preventive strategies, staying informed about HPV, and engaging in honest communication with partners, men can navigate sexual relationships safely. Vaccination, protective measures, and routine health monitoring form the foundation of responsible sexual behavior. Recognizing HPV as a manageable and common infection helps reduce stigma, encourages early detection, and ultimately contributes to healthier communities.
In conclusion, while modern relationship dynamics offer new freedoms, they also demand increased responsibility. HPV represents a significant but often overlooked risk for men, particularly those with multiple se#ual partners. Through education, vaccination, protection, and awareness, men can actively protect their health, minimize transmission, and foster informed, responsible sexual practices. Knowledge and proactive care remain the most effective tools in managing HPV, ensuring that sexual freedom does not come at the expense of long-term well-being.